Fibromyalgia is a chronic pain disorder affecting millions worldwide, including an estimated 10 million Americans. It is characterized by widespread musculoskeletal pain, fatigue, and tenderness in specific areas of the body and can also cause a range of other symptoms. Suffering from this disease can drastically affect your daily life, and getting this diagnosis is hard; it’s crucial to know what the condition entails and when it’s time to visit your healthcare provider to talk about your concerns.

What Is Fibromyalgia?
Fibromyalgia is a chronic health condition characterized by widespread musculoskeletal pain and tenderness, as well as extreme fatigue. It is believed to be caused by the amplification of pain signals in the brain and spinal cord, leading to fluctuating periods of symptoms, known as flare-ups. This means fibromyalgia patients have periods with none (and mild) symptoms and periods with many (and severe symptoms). How long these flareups persist is different for each case. These flare-ups can be emotionally and physically overwhelming for those living with this condition.
Causes & Risk Factors of Fibromyalgia
Medical experts and researchers believe fibromyalgia may be caused by changes in the brain and spinal cord that occur due to repeated nerve stimulation. These changes may involve an abnormal increase in pain-signaling chemicals in the brain and the development of a heightened sensitivity to pain signals in the brain’s pain receptors. The specific factors that contribute to these changes are not fully understood but may include genetic predisposition, infections, and physical or emotional trauma. However, this isn’t the officially determined cause, because there isn’t one yet. What medical experts do know is that there are factors that increase the likelihood of fibromyalgia in people. Risk factors include:
- Gender; women are more often diagnosed
- Hereditary; immediate family members have already been diagnosed
- Chronic illnesses; having osteoarthritis, rheumatoid arthritis, lupus, depression, or irritable bowel syndrome
- Age; people older than 40 are more often diagnosed
- Stress & trauma
Fibromyalgia (flare-ups) can be triggered by various stressors, which can differ from person to person. Some common triggers include emotional stress, changes in daily routine, dietary changes or malnutrition, hormone fluctuations, sleep disturbances, weather or temperature changes, illness, and changes to medication or treatment routine. It is important to pay attention to your own individual triggers and try to manage them as best as possible to reduce the frequency of flare-ups.
Symptoms of Fibromyalgia
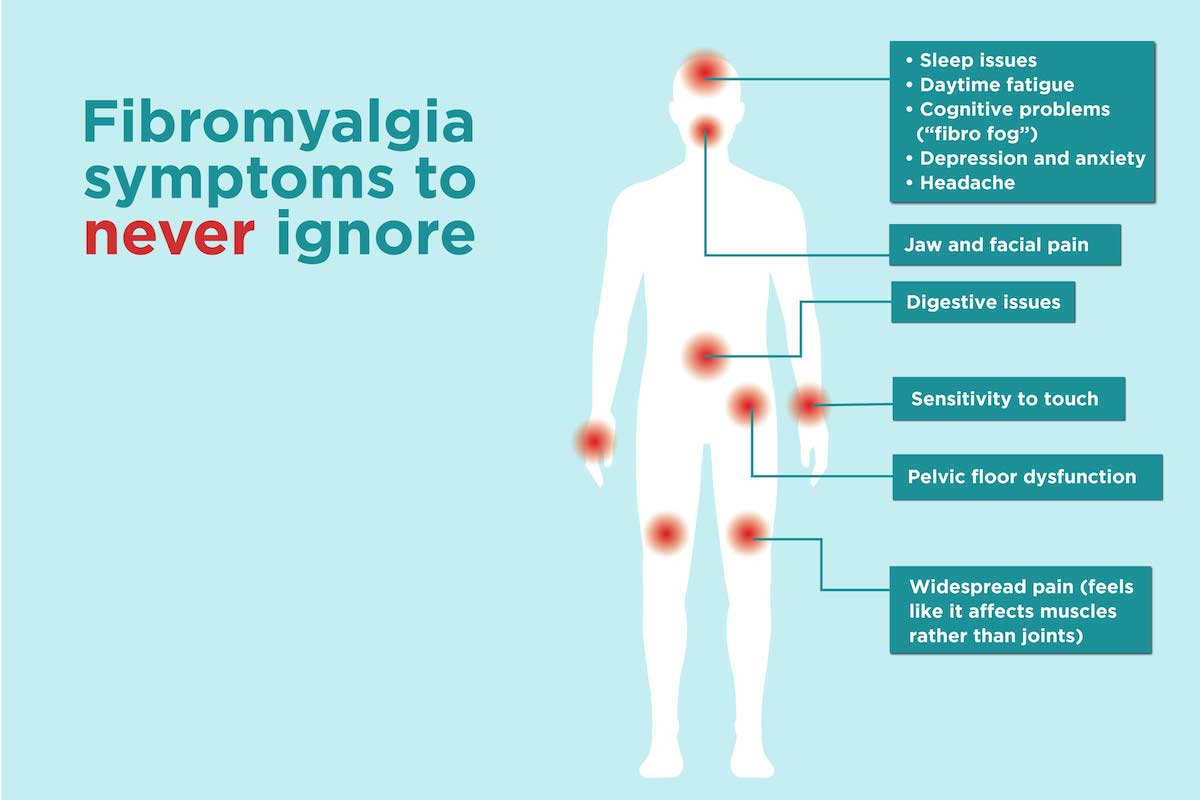
The main symptoms of fibromyalgia include widespread, long-lasting pain, fatigue, and cognitive difficulties such as difficulty focusing and concentrating. The pain associated with fibromyalgia is often described as a constant dull ache and must occur on both sides of the body and above and below the waist to be considered widespread. People with this condition may also experience disrupted sleep due to pain and may have other sleep disorders like restless legs syndrome and sleep apnea. The cognitive difficulties, often referred to as “fibro fog,” can impact daily activities and mental tasks.
Fibromyalgia is often accompanied by other health conditions, including:
- Irritable bowel syndrome
- Chronic fatigue syndrome
- Migraine or other forms of headaches
- Interstitial cystitis or painful bladder syndrome
- Temporomandibular joint disorders
- Anxiety and/or depression
- Postural tachycardia syndrome
- Insomnia and/or other sleep disorders.
Treatment Options
To be diagnosed with fibromyalgia, a person must experience widespread pain throughout the body for at least three months. To meet the diagnostic criteria, pain must be present in at least four of the following five areas: the left upper region (including shoulder, arm, or jaw), right upper region (including shoulder, arm, or jaw), left lower region (including hip, buttock, or leg), right lower region (including hip, buttock, or leg), and the axial region (including neck, back, chest, or abdomen).
There is no one-size-fits-all treatment for fibromyalgia. Which means it’s important to work with a healthcare professional to find a treatment that is effective for you. It is also important to keep your healthcare provider informed of any changes in your symptoms. Including when they improve or worsen. Some treatment options that may be helpful, include over-the-counter or prescription pain medication, exercises such as stretches or strength training, sleep therapy, cognitive behavioral therapy, stress management therapy, and antidepressants.
Unfortunately, there isn’t a cure for fibromyalgia. Treatments will only help to manage the pain and other symptoms. For more information about fibromyalgia and what possible treatment options are, continue your online research here:

