Each year, more than 350 thousand Americans have been admitted to the hospital with pancreatitis. This may not seem like much, but this condition is on the rise. In other words, every year it is (a lot) more hospitalizations. Also in children, and this is worrisome because this condition is rare in children. All this makes it important for everyone to know how to recognize it and what you should do next, in case you have it.
What Is Pancreatitis?
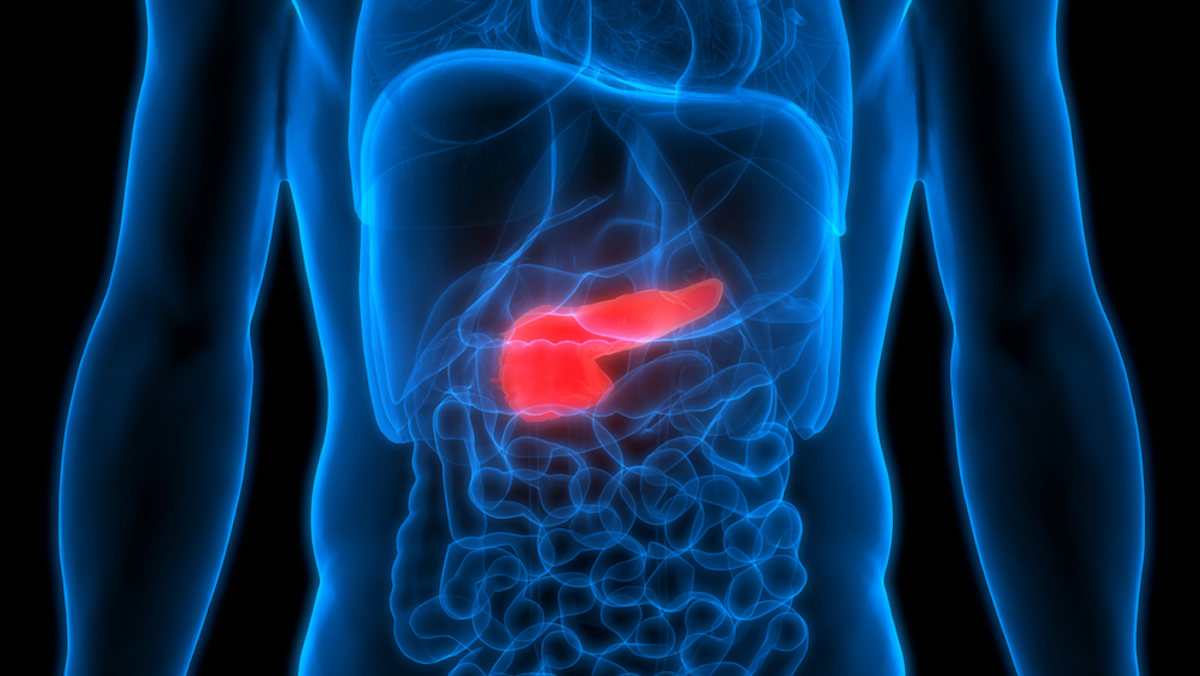
The pancreas is a very important organ, in the upper part of the abdomen, that plays a big part in regulating the body’s blood sugar levels and aiding in food digestion. The organ makes insulin and glucagon, which are vital hormones in controlling the body’s blood sugar. The pancreas also makes powerful digestive enzymes, which it transports to the small intestine, via the pancreatic tube.
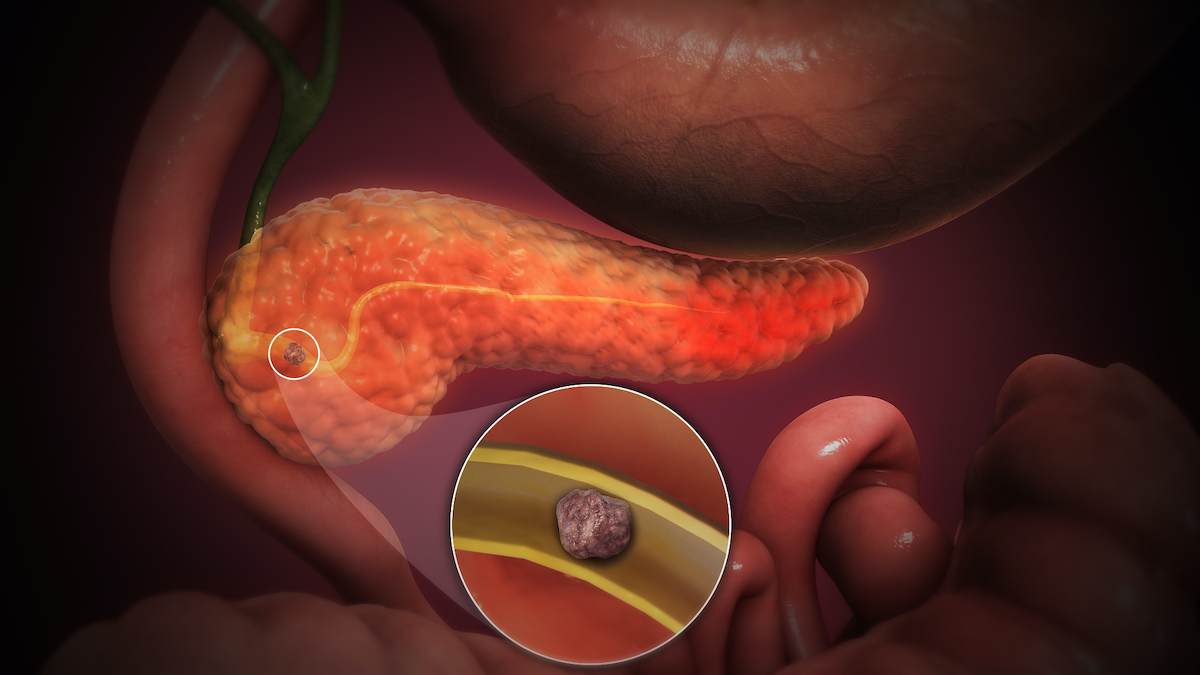
When the pancreas gets irritated and inflamed, it’s called pancreatitis. This occurs when the digestive enzymes become activated in the pancreas instead of the small intestine. The activated enzymes can seriously damage surrounding tissues when the pancreas gets inflamed. In addition, it can release inflammatory cells and toxins that may damage vital organs, like the kidney, lungs, and heart. There are two types, called acute pancreatitis and chronic pancreatitis. Most cases are acute ones, this means that the inflammation of the pancreas is a sudden and short attack. The chronic type is when the pancreas is inflamed ongoing.
Causes of Pancreatitis
There are two main causes of pancreatitis; gallstones and alcohol abuse. Less common causes include:
- Certain medications
- High triglyceride levels
- Infection
- Abdominal injury
- Diabetes and other metabolic disorders
- Cystic fibrosis or other genetic disorders
- Pancreatic cancer
- Obesity
- Trauma
Risk factors that increase the risks of getting this, are excessive alcohol or other substance abuse, smoking, obesity, and being male and/or African-American. Excessive drinking is 3 or more alcoholic drinks per day! Mild to moderate cases can go away with treatment, but untreated or severe cases can have serious to life-threatening complications or even death. These complications include kidney failure, pancreatic cancer, diabetes, internal bleeding, and breathing problems. To prevent these serious health complications, it is important to recognize it and in case you suspect you – or a loved one – are suffering from it, contact your professional healthcare professional as soon as possible.
Symptoms of Pancreatitis
Symptoms of both types can differ. Acute pancreatitis symptoms include:
- Abdominal pain that may spread to the back
- Sudden pain or build-up
- Pain that worsens when eating
- Swollen & tender abdomen
- Nausea & vomiting
- Fever
- Fast heart rate
Symptoms indicative of chronic pancreatitis, which means you do NOT experience them when you have acute pancreatitis, are:
- Constant abdominal pain that radiates to the back
- Unexplained weight loss
- Foamy diarrhea with visible oil droplets
- Diabetes
Treatment Options
Your professional healthcare provider will examine your symptoms and if necessary take some additional tests. These can be an ultrasound, CT scan, stool test, and/or ERCP (endoscopic retrograde cholangiopancreatography). In case you’re diagnosed with this condition, you will be admitted to the hospital for monitoring and appropriate treatment. This consists of pain medication, surgery to remove the cause (such as gallstones) or the part of the pancreas that is too damaged more testing, and possible supplemental pancreatic enzymes and insulin.
Acute pancreatitis normally lasts for a few days to a week, more severe cases can take longer to recover from. Unfortunately, chronic pancreatitis isn’t curable. You will need lifelong treatment when you’re diagnosed with this type. For more information on pancreatitis, the pancreas, and if there are ways to prevent it, continue your online search here:

