Osteogenesis imperfecta, sometimes called “brittle bone disease,” or OI for short, is a rare condition that makes your bones very fragile. Fortunately, It’s not very common in the United States, with only about 1 in 15,000 to 20,000 people having it. This article will explore what causes OI, its symptoms, and its different treatment methods. So, if you or someone you know has OI or wants to learn more about it, keep reading to get all the vital information.
What Is Osteogenesis Imperfecta?
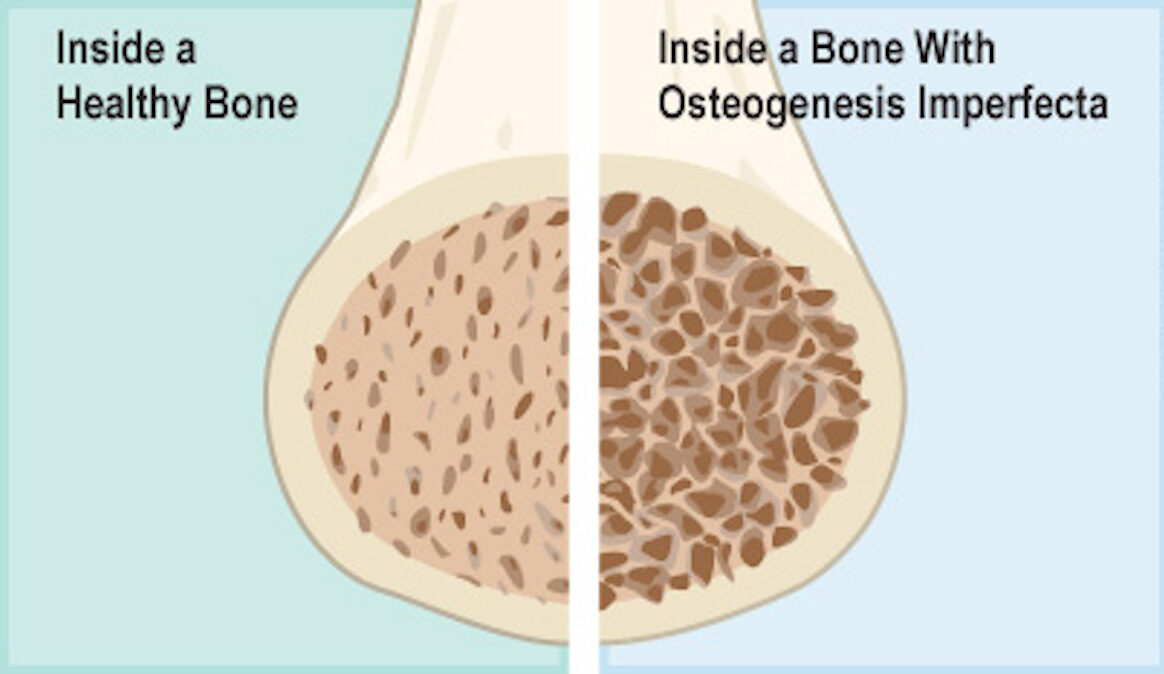
Osteogenesis imperfecta is a rare illness that affects the way your bones grow and stay strong. Imagine your bones are like sticks. In people with this condition, these “bone sticks” are not as tough as they should be. This means they can break more easily than normal, even with small accidents or just by doing regular things. But it’s not just about bones. It can also make your muscles, joints, and other parts of your body not work like they should. Sometimes, it can even affect your eyes. It may come in different types, some more serious than others.
| Type | Description |
|---|---|
| Type I | The mildest form with fewer fractures, near-normal height, and mild bone deformities. |
| Type II | The most severe and often fatal form, with very fragile bones and severe deformities. |
| Type III | Severe bone fragility, multiple fractures from an early age, noticeable deformities, and shorter stature. |
| Type IV | Moderate to severe bone fragility, common fractures, and shorter stature with some deformities. |
| Type V | Similar to type IV but may include "hyperplastic callus formation" after fractures. |
| Type VI | Rare, with bone fragility, fractures, and slower growth. |
| Type VII | Extremely rare, characterized by severe bone fragility, frequent fractures, and delayed bone development. |
| Type VIII | Very rare, involving severe bone fragility and frequent fractures. |
What Causes Osteogenesis Imperfecta?
Brittle bone disease is caused by a genetic issue passed down from parents or occurring as a new change in a person’s genes. This genetic problem affects the production of collagen, a crucial protein for strong bones. When the body can’t make enough collagen, bones become fragile and prone to breaking easily, leading to the symptoms of osteogenesis imperfecta.
People are at risk of having osteogenesis imperfecta if there is a family history of the condition, meaning that their parents or close relatives might have it. Sometimes, OI can also happen when there’s a new change in a person’s genes, even if their family doesn’t have a history of the disease.

Symptoms of Osteogenesis Imperfecta
The two most common symptoms of osteogenesis imperfecta are frequent bone fractures and bone deformities. People with OI often experience frequent bone fractures, even from minor accidents or activities that wouldn’t typically cause broken bones. These fractures can happen in various parts of the body, such as the arms, legs, and spine. This condition can lead to bone deformities, where the bones may not grow or shape properly. Common deformities include curved or bowed limbs and a shortened stature. Other symptoms of osteogenesis imperfecta may include:
- Loose joints: Individuals with OI may have joints that are more flexible than usual, making them prone to dislocations.
- Hearing loss: Some people with OI may experience hearing loss, often due to problems with the tiny bones in the ears.
- Blue or grayish sclera: The whites of the eyes (sclera) may appear bluish or grayish in individuals with OI.
- Dental issues: OI can affect dental health, leading to problems such as weak teeth and a higher risk of cavities.
- Breathing Problems: In severe cases, OI may affect the shape of the rib cage, which can lead to breathing difficulties.
- Heart and blood vessel issues: Rarely, OI can affect the heart and blood vessels, causing complications.
Diagnosis & Treatment Options
Diagnosing Osteogenesis Imperfecta (OI) usually involves a few steps. First, doctors may do a physical exam and ask about any bone fractures or family history of OI. They might also use special tests like X-rays to look at the bones. A blood test can check for certain gene changes linked to OI.
If OI is confirmed, the next step is managing it. There isn’t a cure for OI, but treatment can help a lot. The main goal is to make bones stronger and reduce the risk of fractures. Treatment options may include:
- Physical therapy: This helps improve muscle strength, balance, and mobility, which can protect the bones.
- Medications: Some medicines can boost bone density and reduce pain.
- Surgery: In severe cases or to correct deformities, surgery might be necessary.
- Assistive devices: Using braces, wheelchairs, or other tools can make daily life safer and easier.
- Healthy lifestyle: Eating a balanced diet with enough calcium and vitamin D, not smoking, and avoiding excessive alcohol can support bone health.
Remember, OI varies from person to person, so treatment plans are tailored to each individual’s needs. Regular check-ups with doctors who specialize in bone disorders are crucial to manage OI effectively. The right treatment can really help you feel/get better. Remember: there is no best treatment, only the best treatment that suits you and your symptoms. For more information on OI, other metabolic bone diseases, and possible treatment options, continue your online search here:

