Certain groups of people have a higher risk of contracting Hepatitis C due to their exposure to the virus. Individuals who have injected drugs and shared needles or other drug paraphernalia are at significant risk. Healthcare workers who might be exposed to infected blood through needle stick injuries also face a higher chance of infection. People who received blood transfusions or organ transplants before 1992, when widespread screening of the blood supply was not yet in place, may also be at risk.
Additionally, those who have HIV, received clotting factor concentrates before 1987, or were born to mothers with Hepatitis C, have a higher likelihood of having the virus. Identifying and understanding these risk factors is crucial for preventing the spread of Hepatitis C and for early detection and management.
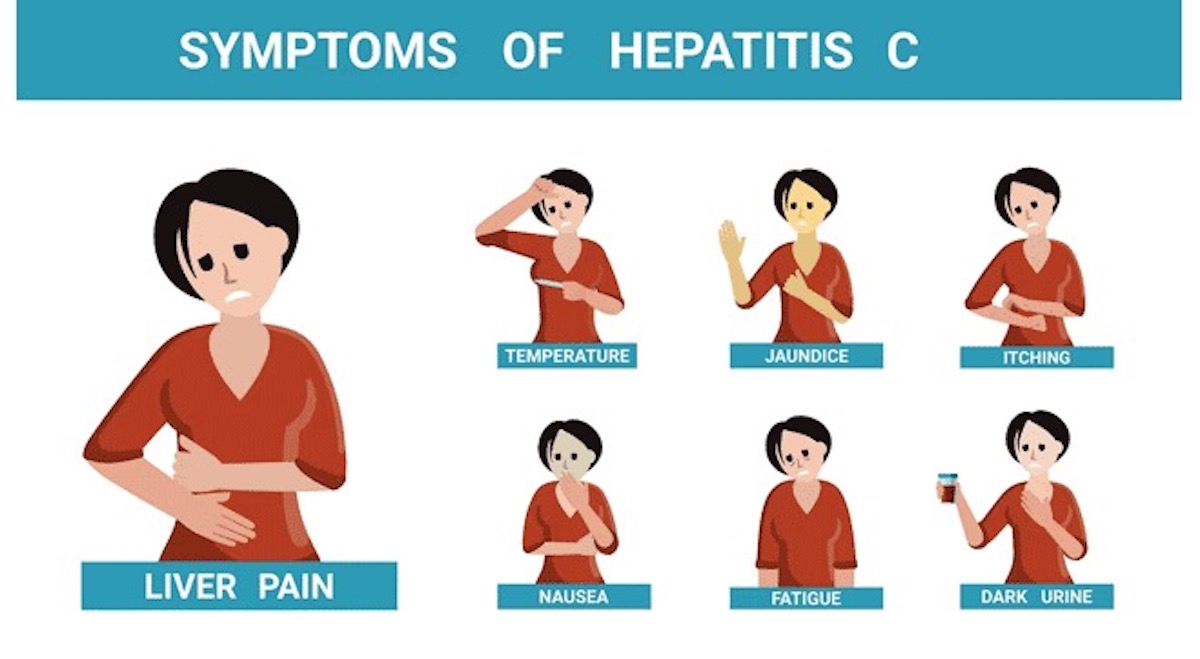
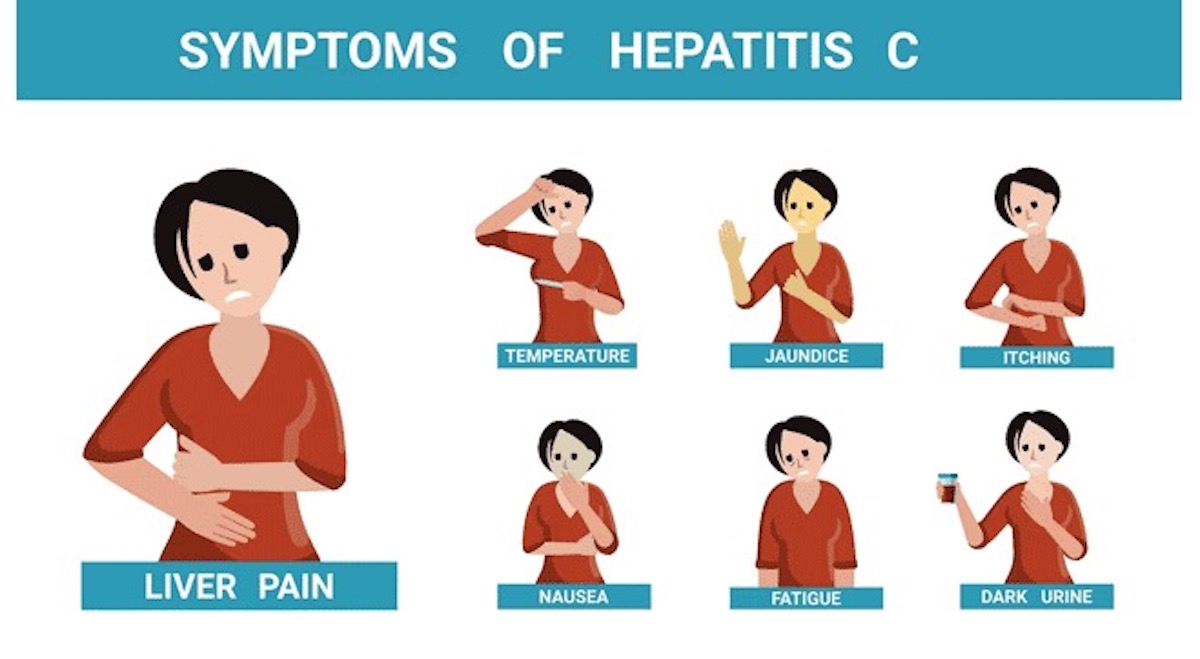
Symptoms of Hepatitis C
Many people with Hepatitis C do not experience symptoms, especially in the early stages of the infection. However, when symptoms do appear, fatigue and joint pain are two of the most common. These symptoms are mostly mild and easily mistaken for less serious health issues. This often leads to delays in seeking treatment. Other common symptoms include:
- Mild fever
- Muscle aches
- Loss of appetite
- Nausea
- Abdominal pain
- Jaundice, which causes yellowing of the skin and eyes
It’s important to be aware of these signs, as they might indicate the presence of Hepatitis C or another liver-related condition.
How Is It Diagnosed?
Doctors diagnose this disease using blood tests that detect the Hepatitis C virus in the body. The initial test, the HCV antibody test, searches for antibodies to the virus, indicating exposure to Hepatitis C. If this test returns positive, doctors then perform a follow-up HCV RNA test to confirm the virus’s current activity in the body. This two-step testing approach ensures diagnostic accuracy and lets healthcare providers determine if a person has an active infection that requires medical attention.
Treatment Options for Hepatitis C
Over the years, treatment options for this disease have significantly improved, now offering potential cures in most cases. The most common treatment employs antiviral medications designed to eliminate the virus from the body. Patients usually take these medications daily for several weeks to months. Another common approach, combination therapy, involves using two or more antiviral drugs to enhance the likelihood of curing the virus. Additional treatment options include:
- Adjusting the treatment plan according to the virus’s specific genotype
- Providing supportive care to manage medication side effects
- Conducting regular monitoring and liver function tests to track treatment progress
These treatments are highly effective and can lead to a complete recovery from the infection. And significantly reduce the risk of long-term liver damage. Need more information? Continue your online search about hepatitis, specifically hepatitis C, here: